17. June 2024
Chronic lymphocytic leukaemia is the most common type of leukaemia in Europe and affects about 600 individuals in the Czech Republic every year, mostly older adults. In an effort to better understand and treat the disease, scientists are creating laboratory models to study this leukemia and test new drugs. A research group led by Prof. Marek Mráz at CEITEC Masaryk University has now succeeded in working with physicians and materials scientists to develop an innovative model that helps to study the mechanisms inducing leukaemia cells proliferation and to identify or test potential new anti-proliferative drugs.
Individuals with chronic lymphocytic leukaemia (CLL) overproduce white blood cells known as B-lymphocytes. These cells are normally part of the immune system and help the body fight infections by producing antibodies. However, in CLL, B lymfocytes multiply uncontrollably and cause the immune system to weaken. Patients may then be more susceptible to infections, feel tired, and suffer from anaemia or increased bleeding because the abnormal B-lymphocytes gradually suppress the healthy haematopoiesis in the bone marrow.
Targeted drugs aimed directly at the tumour B-lymphocytes are commonly used to treat CLL, but over time the malignant cells become resistant to the treatment. One major problem in the development of new drugs is that leukaemia cells do not multiply in laboratory conditions as they do in the human body. They lack the supportive microenvironment of the patient's lymph nodes, where they come into contact with other non-malignant immune cells essential for aggressive tumour behaviour. Scientists are therefore trying to simulate the supportive microenvironment laboratory conditions to study the process of cell division (i.e., proliferation) and to effectively test the efficacy of newly developed drugstest the efficacy of newly developed drugs. However, the models available so far are not very effective in inducing proliferation and are costly, as they require replacing natural interactions in the patient's body with laboratory-prepared proteins.
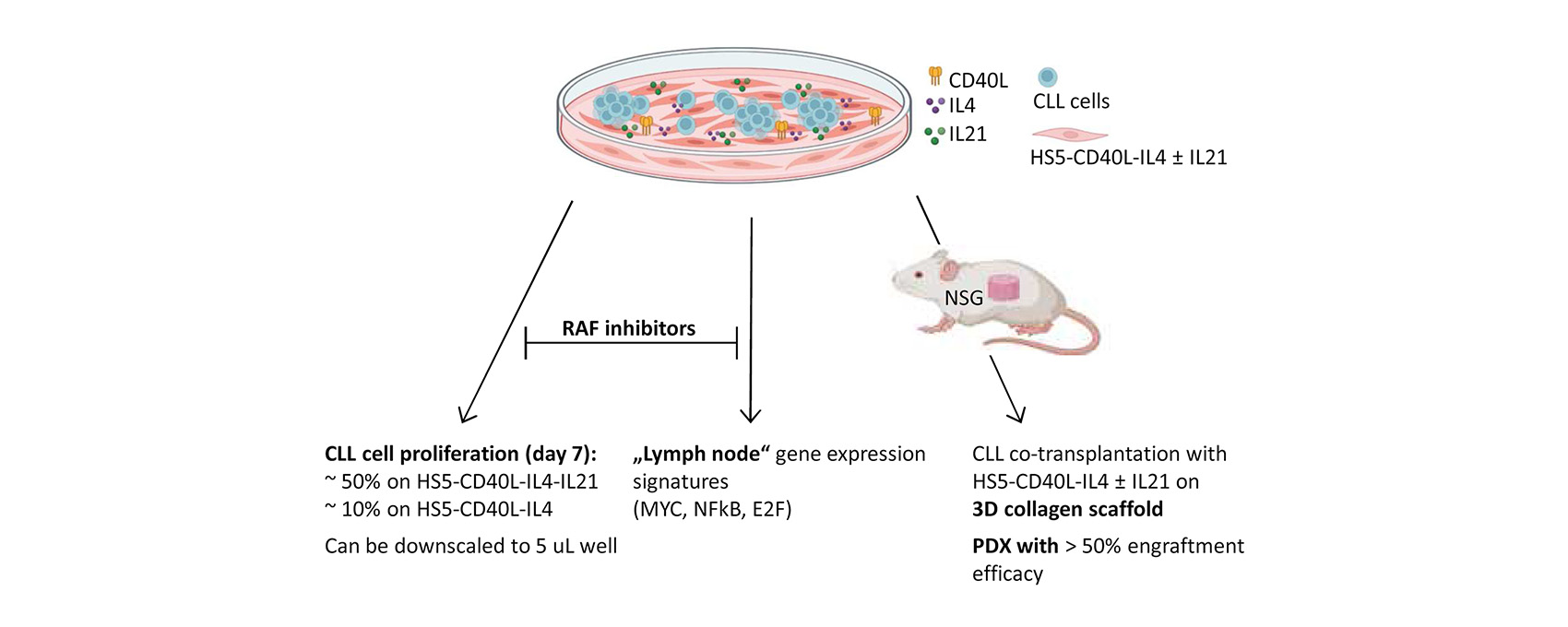
A research team consisting of scientists from CEITEC Masaryk University, University Hospital Brno, Faculty of Medicine Masaryk University and CEITEC Brno University of Technology has now developed an innovative model of a supportive microenvironment that enables a highly efficient proliferation of leukaemia cells in laboratory conditions. It contains bone marrow cells that are modified to produce proteins (called cytokines) required for leukaemia cell growth. "These cells have been genetically modified to promote the proliferation of CLL cells in in vitro cultures. This eliminates the need to add artificially produced cytokines, which are very expensive," says Eva Hoferková, first author of the study. "Thanks to this model, we have, among other things, described for the first time that inhibitors of the RAF kinase family can effectively stop the proliferation of CLL," she adds.
An important aspect of the study, which was published in the prestigious journal LEUKEMIA, was the long-term collaboration with scientists from CEITEC Brno University of Technology, which enabled the model to be tested in mice. The students in Prof. Lucy Vojtová's laboratory prepared special scaffolds, tiny porous cylinders made of collagen, which can be embedded with modified support cells and inserted into the subcutaneous tissue of the mouse to artificially create a microenvironment for the growth of leukaemia cells.
"By co-transplanting supportive cells on the scaffold and CLL cells, we achieved engraftment and growth of leukaemia cells that does not otherwise occur in mice. This procedure enables the creation of a ‘patient avatar’, i.e. theoretically we can use the cells of any patient to prepare a mouse that can be used, for example, for drug testing," comments Prof. Marek Mráz, the leader of the study.
The project has been supported by funding from the Jaroslav Koča Bridge Fund, which encourages interdisciplinary collaborations at the interface of life and material sciences at CEITEC, and co-funded by the National Institute for Cancer Research (NICR).


 Share
Share