23. July 2024
Cancer is the leading cause of death worldwide. According to alarming expert predictions, its incidence is expected to rise by almost half within 20 years. The main problem is not the aggressive growth of cancer itself, but rather the invasion and metastasis that are responsible for most deaths. A research project led by Daniel Zicha within the Experimental Biophotonics research group and the Biophotonics Core Facility at CEITEC BUT is therefore investigating whether some of the drugs approved for other purposes have the side effect of slowing or even stopping the spread of cancer cells.
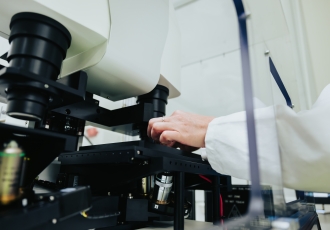
For this purpose, they use a holographic microscope that allows them to follow the migration of these cells with high precision. The advantage of using already approved drugs is that they can be given to the patient immediately, bypassing the lengthy approval process.
You are collaborating with the BIOCEV Centre on a project funded by the GAČR; how did you come to it?
I have been working on this topic since 1985, so for forty years. My colleagues at the centre and I have a common interest in the study of metastasis, and our scientific approaches, such as light microscopy, overlap. We complement each other, and our collaboration has led to the idea of applying for a grant. At BIOCEV, they focus on 3D fluorescence methods, while we use 2D holographic interference microscopy for quantitative phase measurements. This technique allows us to measure cell behaviour more accurately, albeit on a smaller scale. What it means is that they do the larger screening, pick out the candidates for us, and we verify them in detail. We then delve into researching the mechanisms – how it works.
When we talk about holographic imaging, should I think of it as showing you the tumour? Do you see a hologram of it?
A tumour is three-dimensional; we can’t do that routinely yet. What we can do very well, however, is image individual cells that are detached from a tumour fragment and are on a solid substrate – a coverslip. The cell is spread out and we image it in a two-dimensional projection. We can see the exact contours, the distribution of the mass, and thanks to this microscopic method, which is compatible with living cells, we can observe their dynamics – how the cell moves and divides. Since we measure the mass distribution with precision, we can integrate the total mass of the cell and see how it grows and increases in mass.
You want to use drugs for this research that are used to treat other diseases. How many are you going to test? And what types?
Since both groups have been working on the topic of cancer cell migration for a long time, we know from the literature and our own research what the molecular mechanisms required for migration are. We have, therefore, tried to identify drugs that have at least some indications or are known to influence these processes. We have also consulted with pharmacology experts. We have identified 180 drugs, some of which are more likely to be effective, others less so. If the project is successful, we can expand the study.
Why have you decided to test drugs that are already approved?
There are cases where some drugs have been shown to have positive effects beyond what they were primarily intended for. For example, the drug Antabuse, which was originally developed to treat alcoholism, has side effects that are now used to treat cancer. This principle is well known and has benefited mankind on several occasions. The concept of using drugs to influence the migration of cancer cells came from our collaborator, Professor Jan Brábek. He coined the term migrastics, analogous to cytostatics. Professor Brábek came up with the term and is the leading figure in this field. We are co-investigators in the project.
At what stage is the research?
We have already started testing the drugs –we are first testing them on established cell lines that are easy to work with. These are cancer cells that were taken from a patient a long time ago and are established in cell culture, so they are immortal and grow pretty much all the time. Now, for example, we’ve worked with tumour cells from the 1970s.
So, the aim of the project is not to destroy the tumour with drugs but to slow down, ideally stop, the spread of the tumour and, therefore, the formation of metastases?
Exactly. As far as I know, this is the only project, which is surprising because it’s quite a simple idea, and very useful! Once we find something, the doctor can immediately give it to the patient. We can avoid that lengthy process of approving a new drug, which would take 10, 15 years and millions and millions of dollars.
Why are you focusing on metastasis?
When the cells are just dividing, growing, and forming new ones, the tumour only gets bigger in one organ in one location. This scenario is less dangerous for the patient, and the surgeon can address it by removing the tumour. The most dangerous scenario, which kills most patients with tumours, is metastasis. When the tumour begins to spread, the surgeon can no longer remove all of the metastases, especially if they are scattered and diffuse. That is why we are focusing on the migration and spread of tumour cells in our project; this is not sufficiently taken into account in treatment. It is surprising that all the development of chemotherapy is focused on stopping cell division and destroying cells, but no one cared whether the drugs affect migration. And no one cares even today, which is surprising but, unfortunately, true. It is much easier to develop something that will kill a cell than something that will affect its migration because you need a very subtle intervention. It’s not like hitting a cell with a hammer to make it die. It only takes a small modification to make the cell move slower or faster.
So these drugs could be used as supportive therapy? The patient finds out he has a tumour and starts taking the drugs to prevent its spread?
Yes, that’s the idea. And it could also be the other way around, that existing treatments would complement this important aspect because metastasis is more dangerous and can actually get worse during standard treatment. The surgeon doesn’t know exactly how far the tumour extends in surgery. He tries to remove as much as possible but mustn’t affect important organs nearby. So, there may be some cancer cells left behind. The operation creates a wound, like a knife cut at home. The wound has to heal, which stimulates the proliferation and migration of cells to heal the wound. However, this healing process is bad for a person with cancer because if any cancer cells remain, they will be further stimulated to grow and migrate. So, if we had a drug that would stop the migration, it would certainly be interesting to cover the surgery with it. Maybe administer it before the surgery.
How do you ensure that the drugs target the migration of cancer cells, not healthy ones?
That’s the subject of our research. Because it is an approved drug, we know that it will not have a dramatic effect on the migration of the cells that we want to migrate. Migrating cells in the body are primarily part of the immune system. When an infection gets into a wound, white blood cells have to come in to clean it up. We don’t want to inhibit the white blood cells, which unfortunately chemotherapy does because it kills them. White blood cells are cells that rapidly divide in the bone marrow, and chemotherapy destroys them. It’s basically a game of whether the patient or the tumour lasts longer. And this might be less drastic.
Do all cancers migrate the same way? Or will it be necessary to target different drugs for each type?
It could be different because cancer is a collection of diseases that have common features but also some differences. So specialisation is to be expected. Potentially different combinations of drugs could be needed. Everything is moving towards personalised treatment, which is another huge field we would like to enter in the future – where you find out what type of tumour it is, what type of person it is (= genetics) and prescribe a cocktail of drugs. In the meantime, we want to record some basic, general mechanisms that would cover a fairly large proportion of cases.
You are the head of the new Biophotonics Core Facility at CEITEC BUT. What makes it special?
Our main instrument is a holographic microscope with an incoherent light source. This means that the source is not a laser as in the case of cheaper versions, but an LED illuminator, which allows for interference images more precise than in the case of a laser. This is key to eliminating the effect of dust and optical inaccuracies on the final image. This unique microscope developed in Radim Chmelík’s laboratory is the only one of its kind in the world. We have been using it since the first prototype and are now working with the latest model, which is also used in Prague, Germany, England and Greece. In the group, we are interested in living cells – how they behave and migrate. Our lab is also a service lab, we support other people’s projects, too, both in the academy and the commercial sphere.


 Share
Share